Diagnosis and treatment with hemangiom in children.
The content of the article
- Hemangioma in children, newborns, chest: what it is, what does it look like, views?
- What does hemangioma look like?
- Types of hemangiom in children on the face and on the body: internal, subcutaneous, capillary, cavernous, combined, mixed
- Gemangioma in a child: signs and causes of occurrence
- Gemangioma in children: is it dangerous to what age is growing to?
- To which doctor to contact the hemangioma in a child?
- The child grows Gemangioma - what to do?
- Hemangiom treatment in children
- Surgical removal of hemangioma child with a laser, liquid nitrogen: indications, consequences
- Is Propranolol and Timolol with hemangioma are effective?
- Conspiracy from hemangioma in children
- Gemangioma in children: reviews
- Video: Dr. Komarovsky about hemangiomas. What tactics of treatment should choose and why?
Hemangioma in children, newborns, chest: what it is, what does it look like, views?
Hemangioma is a vascular neoplasm, a benign tumor. Most often detected in newborns or during the first year of the life of the baby (in 10 percent of children).
Medicine is known for the development of hemangioma and at a later age.

Infant hemangioma in a century
What does hemangioma look like?
The hemangioma and mucous eye visible on the skin and mucous eye looks like a bug-noded, a bug-and-flat formation of red or bluish-red color with clear edges.
- Tumors can be both flat, leather and slightly protruding over it.
- Subcutaneous hemangiomas look like swelling, without characteristic color changes on the cover of the body.
- Internal hemangiomes are invisible without special equipment.

Capillary Hemangioma Hospitally
All varieties of hemangiom on external features are conventionally divided into types:
- Star
- Shishkovoid
- Venous
- Fire Nets

Star Gemangioma
Types of hemangiom in children on the face and on the body: internal, subcutaneous, capillary, cavernous, combined, mixed
A more detailed classification, taking into account both the composition, and the external manifestation of hemangioms on the face and body of the child at the same time, is presented below.
- Internal. Located in organs (liver, brain, ovaries) and bones, do not have external manifestations.
- Subcutaneous. There are no boundaries on the skin, while the body of the tumor is located in the subcutaneous fiber layer.
- Skin
- Capillary (vascular). Externally flat, pale when pressing.
- Cavernous. Consists of cavities (cavities) filled with blood. Convex, increases with or cough, falls as pressing.
- Combined. Includes vascular component and cavity.
- Mixed. Combines in its composition and cavity, and capillaries, as well as tissues of other types (connective, nervous).

Subcutaneous infant hemangioma
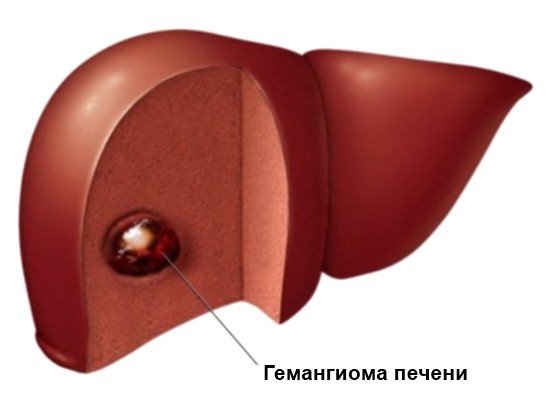
Hemangioma liver (scheme)
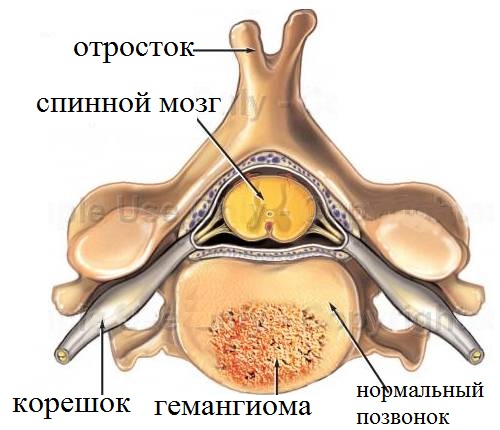
Spinal hemangioma (scheme)
Gemangioma in a child: signs and causes of occurrence
For proper diagnosis of hemangioma, a combination of all characteristic features is necessary:
- In the first time, the tumor develops quite quickly, increases in size, due to which hemangioma can be distinguished from, for example, the godded stain.
- Thanks to the large influx of blood in the hemangioma vessels, it is hot, than those surrounding her fabrics.
- When pressing a tumor pale, after stopping the impact quickly restores the original color.

Combined hemangioma in the field of breast
Most often, hemangiomas are located:
- on the skin of the head (eyelids, cheeks, nose, hairy part, headings)
- on the skin of the limbs (Hand brushes, soles legs, buttocks)
- on the body (belly, back)
- on mucous membranes (nasal paths, mouth cavity, genitals)
- on internal organs (liver, spleen)
- on the organs of the musculoskeletal system (Bones pelvis, skull).
An unequivocal answer to the question why this is often found this benign tumor and how to prevent its appearance does not exist.
Since in the overwhelming majority of cases, Gemangioma manifests itself in a child from birth or at the breast up to a year, it is believed that the main reason is an anomalies for the development of the vascular system in the embryonic period. At the same time, experts also note the dependence on the gender of the baby, since in 80% of cases of hemangiomas arise from girls.

Multiple hemangiomas on the leg and body of a newborn
Other probable reasons that increase the risk of hemangioma in children:
- viral diseases transferred during pregnancy
- heredity
- unfavorable environmental situation
- mature mother age
- alcohol Abuse, Smoking
Gemangioma in children: is it dangerous to what age is growing to?
One of the distinguishing features of hemangioma in children is the presence of two main phases of development.
- Stage of height. It lasts, as a rule, for 6-12 months, as a result of which the tumor reaches its final size.
- Stage Regress (involution). This is a poorly learned process of reverse development of hemangioma, leading to the complete disappearance of the neoplasm, the reasons for which are still unknown.
Given these features, the overwhelming majority of surgeon doctors recommend parents to apply expectant tactics in the treatment of hemangioma in children.
In 90% of cases, the tumor passes without a trace to 7 to 9 years.
However, late treatment can lead to hemangioma growth with the subsequent destruction of organs, muscles, bones and nearby fabrics, serious cosmetic problems, the cultivation of the tumor in malignant.

Subcutaneous hemangioma in the age of
The injury of hemangioma causes bleeding, which is difficult to stop.
To which doctor to contact the hemangioma in a child?
The treatment of hemangi, as well as other tumors, is engaged in a surgeon of general practice. In difficult cases, additional consultation of a highly specialized surgeon (maxillofacial, plastic), as well as a cardiologist may be required.
The child grows Gemangioma - what to do?
As noted earlier, tumor growth in the first 6 - 12 months after the appearance is the norm. The expectant tactic does not apply if the following signs are characteristic of hemangioma:
- Excessive and long-term growth. Parents can track this parameter independently, periodically photographing the neoplasm and measuring its size. The testimony for treatment is the growth of the tumor after a two-year-old child.
- Hemangioma development on centuries, near the physiological holes, in traumatic places.
- The formation of hemangioma on internal organs and bones. Such a tumor does not allow the children to develop normally.
- Large sizes of tumorcreating a significant cosmetic defect.

Capillary hemangioma on the face requiring operational treatment
note: Physiotherapeutic procedures can provoke further hemangioma growth. Apply them only in case of extreme need!
Hemangiom treatment in children
First of all, a complete examination of the child is carried out, the purpose of which is to determine the type of tumor, its structure, sizes and potential hazards in its further development. For this purpose, a complex of laboratory and instrumental research is appointed:
- General blood analysis for reducing the levels of platelets and hemoglobin in the blood circulating in vessels of tumors
- ultrasound - to determine the type of hemangioma
- CT, MRI, thermography - to establish the true size of hemangioma
- Angiography - investigation using injected contrast agent into the vessels, wherein the determined level of involvement of other organs tissue growth hemangioma; used in difficult cases that require surgery, for example, the bones of the skull.
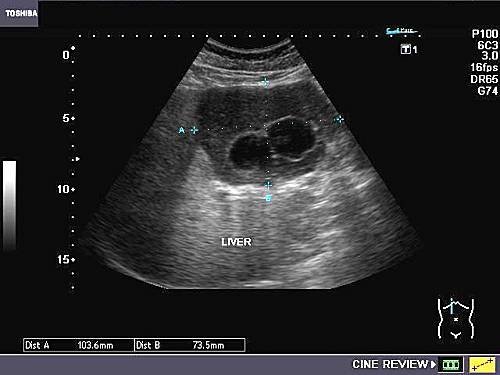
Multiple hepatic hemangioma (US)
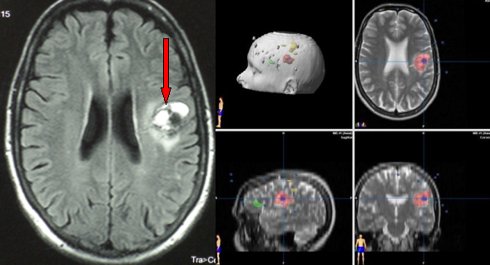
Cavernous hemangioma of the left frontal lobe of the brain (MRI)
According to the research doctor chooses the tactics of temporizing or surgical treatment. In modern medicine, used the following methods of dealing with hemangiomas in children:
- cryolysis - Freezing tumors with liquid nitrogen.
- Exposure to the laser - laser destruction of tumor vessels.
- electrocautery - cauterization using an electric current. It can be used with any form of surface hemangioma.
- sclerotherapy - administering injections with a special composition, the sealing vessels.
- Radiation therapy - removal of the tumor directed x-rays. Used when hemangiomas internal organs, bones, or inability to use another method (e.g., if the tumor is located in the orbit).
- Operation - method inefficient and traumatic, which often have seen the development of hemangiomas in neighboring areas. It is used only in extreme cases.
- medication - treatment with drugs, having in its composition timolol, propranolol, hormones.
Self-treatment of hemangiomas in children is not recommended!
Surgical removal of a hemangioma laser child with liquid nitrogen: indications, consequences
Removal of liquid nitrogen hemangioma applied at any stage of the development of cutaneous hemangiomas, but only small sizes.
- Produced for 1 - 4 sessions, with the consequent formation of crusts on the surface treated with nitrogen.
- Desirable when cavernous, combined and mixed type, as freeze-deeper tissues probably appearance of rough scars.

Combined hemangioma after one session cryoablation. Light areas - the scar tissue.
removal by laser - it is almost painless method that does not require a long rehabilitation.
- The laser can influence the hemangioma dot without touching or damaging the surrounding tissue.
- surface of the skin after the treatment does not scar.
- However, this method is characterized by the multipleness and duration of sessions.
- Like the cryodestruction, the removal of the laser is successfully applied in cases of capillary hemangioma, or in a complex with other methods of treatment.

Hemangioma Laser Removal Result
Is Propranolol and Timolol with hemangioma are effective?
Treatment with preparations containing propranolol and thymolol is a pretty new method of combating infant hemangiomas.
Propranololespecially effective with cavernous and internal hemangiomas. Preparations with propranolol (most often Anaprilin) \u200b\u200buse with to remove such tumors since 2008.
- Propranolol is taken inside for 6 - 12 months.
- Saving vessels, it is able to stop tumor growth and launch regression mechanisms, but it is impossible to take such drugs.
- An individual dose is calculated only by the attending physician, taking into account the view of the cardiologist, since the main action of propranolol has on cardiac activities.
- On the contrary, insufficient reception of the drug will not be expected to therapeutic effect on the development of the tumor.

Effect after hemangioma treatment with propranolol
Timolol It is part of the eye drops and gel against glaucoma. The therapeutic effect in combating skin hemangiomas was revealed by chance in 2010.
- The drug containing thymolol is rubbed into the tumor every 8 hours for 2 to 3 months with interruptions in 1 - 2 months to avoid addiction.
- Tale of the neoplasm is noticeable after 2-3 weeks of application.
Conspiracy from hemangioma in children
If traditional treatment methods do not help, or the disease returns again and again, hitting the neighboring parts of the body, you can try using white magic conspiracy.
It is necessary to sprinkle a thread of sheep wool and tie seven knots on it. For each node to boil:
- warm, flesh,
- tears, blood,
- morning,
- day,
- night,
- trouble stand
- go away.
After that, the thread must be tied to the Suc of Osin growing in the forest.
Gemangioma in children: reviews
- Most parents note that the most affordable method of fast struggle with hemangioma in children in Russian hospitals remains cryodestruction. However, a large minus with this method is the scarring of the skin surface.
- Laser therapy - Really highly efficient, but costly. At the same time, laser equipment necessary for it is often located only in large cities.
- medication Practically does not leave cosmetic defects, but you need to be prepared for the duration of treatment and the regularity of drug reception.

Hemangioma on the nose after drug therapy
From how promptly parents will turn out for help to a competent specialist depends primarily in the child's health. In the overwhelming majority of cases, hemangiomas are succumbed to successful treatment without complications and significant skin defects.